Is a WATCHMAN Implant right for your patients?
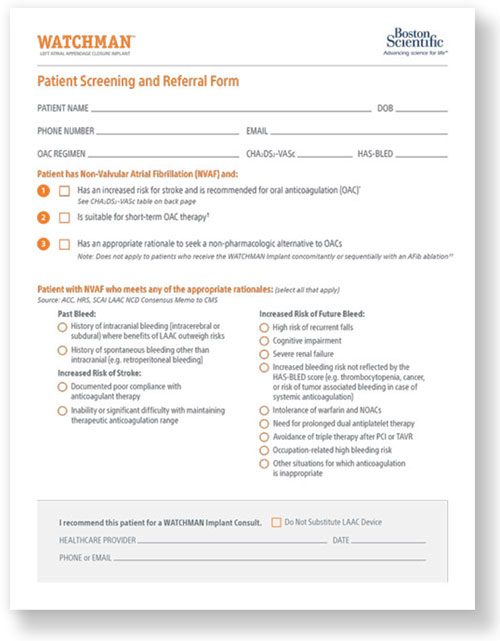
WATCHMAN Implant candidates may include a broad range of patients who:
- Have an increased risk for stroke and are recommended for oral anticoagulation (OAC)
- Are suitable for short-term OAC*
- Have an appropriate reason to seek a non-pharmacologic alternative to OACs
Note: Does not apply to patients who receive the WATCHMAN Implant concomitantly or sequentially with an AFib ablation†
The CMS National Coverage Determination (NCD) remains unchanged. The patient must be deemed unable to take long-term OAC and meet all criteria in NCD 20.34 to be eligible for coverage.
See examples of patients who may be appropriate WATCHMAN

Case study 1: Patient with previous major bleeding
Patient history
- 75F
- Patient has prediabetes, paroxysmal AFib, hypertension, CHA2DS2-VASc: 6-7, HAS-BLED: 4
- Year 1: Diagnosed with AFib, started apixaban 5 mg, twice a day
- Year 2: AFib ablation
- Early Year 3:
- Foot drop→ First hemorrhagic stroke
- CT scan found a hemorrhagic lesion
- Apixaban discontinued
- Late Year 3: Headache, loss of balance→ Second hemorrhagic stroke in same vascular bed
- During hospitalization, patient had pulmonary embolism (PE) and had an IVC filter (could not get anticoagulation due to recent hemorrhagic stroke)
Clinical Challenge
Patient is at risk for stroke, has had a major bleeding event more than once and will not be able to withstand long-term systemic anticoagulation.
Patient criteria and therapy decision
Patient meets the criteria for having had a previous bleed, in this case a major bleed, and was deemed suitable for post-implant dual antiplatelet therapy (DAPT) by an interdisciplinary care team. Therefore, patient should be considered for WATCHMAN.

Case study 2: Patient with multiple conditions prohibiting anticoagulants
Patient history
65M
Patient has AFib, atherosclerotic cardiovascular disease (ASCVD) (carotid, coronary, peripheral artery disease), hypertension, obstructive sleep apnea on CPAP and an aortic aneurism who presents for follow up of more frequent palpitations
Holter Monitor: ~20% burden of AF/AFL, longest episode duration of 12 hours and 22 min, fastest heart rate 169 bpm. Patient events correlated with mostly AF/AFL
Meets indication for "secondary" prevention ASA 81 mg given multiple vascular beds with ASCVD
Patient had severe epistaxis last year on apixaban requiring multiple ER visits to stop the bleeding. He is currently not on anticoagulation because of this.
Clinical Challenge
Patient has concomitant medications and has had a minor bleed that could be considered significant. He should not be rechallenged with another anticoagulant, or discontinue aspirin, because of his vascular disease.
Patient criteria and therapy decision
Patient has a history of minor bleeding and comorbidities that require treatments that may not be compatible with OAC
Patient can be considered for WATCHMAN based on bleeding history and clinical risk factors

Case study 3: Patient at risk for future bleed
Patient history
75M
Patient has chronic, persistent AFib (CHA2DS2-VASc=7), prior cerebrovascular accident (CVA), diabetes, coronary artery disease (CAD) after silent myocardial infarction (MI) who presented from his PCP
Had a CVA when he was off OACs for ENT surgery five years ago
Labile INR with time in therapeutic range 20%
Frequent falls
Unable to afford apixaban
Clinical Challenge
Patient has a history of falls with low time in therapeutic range, and also struggles to afford his medication.
Patient criteria and therapy decision
The patient has frequent falls, low time in therapeutic range, is considered at high risk for future bleeds, and is appropriate to consider for WATCHMAN.

Case study 4: Non-compliant patient
Patient history
77M
Cigar smoker with history of mucosa-associated lymphoid tissue (MALT), prediabetes, hypertension (HTN), AFib on flecainide, sleep apnea, remote gastrointestinal bleeding, s/p implantable loop recorder (ILR) and GERD, presents for evaluation of post-COVID shortness of breath.
Only taking ASA 325 mg
CHA2DS2-VASc=4 (Age, HTN, non-obstructive coronary artery disease (CAD))
Meets criteria for OAC, but declines
Clinical Challenge
Patient is at risk for stroke but declines OAC.
Patient criteria and therapy decision
This patient struggles with OAC compliance but is at risk for stroke and is therefore appropriate to consider for WATCHMAN.
Case descriptions are for educational purposes only; not real patient cases.
For full information regarding WATCHMAN patient selection factors, please see the WATCHMAN Device Directions for Use (DFU).
Learn which of your non-valvular AFib (NVAF) patients may be eligible for WATCHMAN
* Option for immediate DAPT-only post-implant drug regimen for standalone WATCHMAN procedures.
† In the OPTION trial, sequential LAAC was a minimum of 90 days post AFib ablation (as a protocol-driven blanking period).
References:
1. Boston Scientific Corporation. (2018). WATCHMAN Salesforce Database. N=19,000.
