The WATCHMAN Implant procedure is a one-time procedure that helps lower your stroke risk with atrial fibrillation (AFib) not caused by a heart valve problem. It’s an alternative to blood thinners for people who need one. The WATCHMAN Implant works by sealing off the left atrial appendage (LAA), a small area in the upper chamber of your heart and forming a barrier to blood clots. The WATCHMAN Implant stays in place permanently. Once the LAA has healed, most people can stop taking blood thinners to reduce their risk of stroke with AFib.*1 In this article, we’ll explore what to expect after the WATCHMAN Implant procedure.
There are risks associated with all medical procedures. Please talk with your doctor about the risks and benefits of the WATCHMAN Implant.
What happens after the WATCHMAN Implant procedure?
A doctor places the WATCHMAN Implant into the LAA of your heart using a long, thin tube (called a catheter) through a small incision in your upper leg. This is considered a minimally invasive procedure.
After the WATCHMAN Implant procedure, your own heart tissue will begin to grow over the device, closing off the LAA. That’s why the WATCHMAN Implant procedure is also known as an LAA closure. Since 90% of stroke-causing blood clots are formed in the LAA, closing it off with the WATCHMAN Implant is an effective way to reduce your risk of stroke.2
What is recovery like after the WATCHMAN Implant procedure?
After the WATCHMAN Implant procedure, most people stay in the hospital for one day or less. After a few days of recovery at home, many people can start to gradually return to their daily activities or to work. However, check with your doctor before participating in any strenuous activity after your procedure.
Follow-up visits and testing after the WATCHMAN Implant procedure
The WATCHMAN Implant procedure is a one-time procedure. It is a permanent implant and doesn’t ever have to be replaced. However, you’ll have follow-up visits and tests to monitor how your heart tissue is growing over the WATCHMAN Implant to create a barrier against blood clots. Most people will have post-procedure follow-up appointments 45 days, 6 months, and 12 months after the procedure.
At your follow-up appointments, your doctor will use imaging tests to take pictures of your heart to check your progress and see if there are any leaks.
What imaging tests do you need after the WATCHMAN Implant procedure?
There are two types of imaging tests doctors can use to check your progress — a computed tomography (CT) scan and a transesophageal echocardiogram (also referred to by the medical abbreviation TEE). These imaging tests allow your doctor to check on your device and make sure that your LAA is sealed.
What is a CT scan?
A CT scan is a non-invasive imaging test that uses a series of X-rays to create an image of your heart.3
What is a TEE?
A TEE is an imaging test that uses sound waves to create an image of your heart. For this test, your doctor will guide a thin flexible tube down your throat into your esophagus (the tube that connects your mouth to your stomach). At the end of the tube, there’s a transducer that makes the sound waves that create the image. Since the esophagus is closer to your heart, a TEE can give your doctor a more detailed view of how well your heart is healing after the WATCHMAN Implant procedure.4
Medication adjustments after the WATCHMAN Implant procedure
After the WATCHMAN Implant procedure, your doctor will prescribe a medication regimen that’s best for you. You’ll need to take your medications until your LAA is completely closed off.
Most people will take one of two options:
- Option A — You’ll take a short-term blood thinner (anticoagulant) for 45 days, followed by an antiplatelet medication and aspirin until 6 months post-procedure.

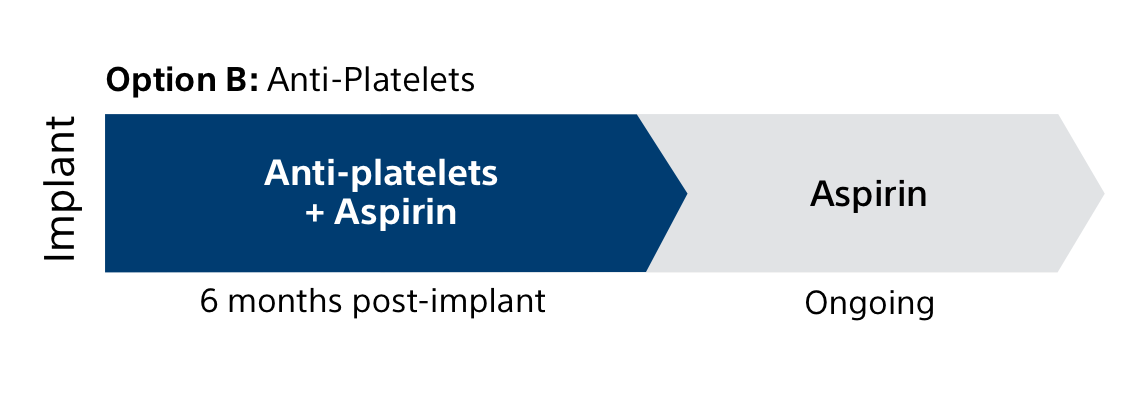
- Option B — You’ll take an antiplatelet medication and aspirin for 6 months.
When can you stop blood thinners?
At your 6-month appointment, your doctor may stop your antiplatelet medication. However, most people will continue to take aspirin on an ongoing basis.
In a clinical trial, 96% of people stopped their blood thinners 45 days after getting the WATCHMAN Implant procedure.1
Learn more about how blood thinners work.
Find out if you’re a candidate for the WATCHMAN Implant. Take the quiz
Does the WATCHMAN Implant cure AFib?
It’s important to remember that, like blood thinners, the WATCHMAN Implant doesn’t cure AFib. You’ll need regular follow-up visits with your doctor to monitor your AFib and your overall health.
After the WATCHMAN Implant procedure, most people can stop taking blood thinners. If you’re taking other medications for AFib or another medical condition, it’s important to keep taking your medications exactly as prescribed.
What is the WATCHMAN Implant card?
On the day of your WATCHMAN Implant procedure, you’ll get a WATCHMAN Implant card. Once you get this card, you’ll carry it with you at all times. That even includes times you step out for a quick errand. It’s important to keep this card with you because in an emergency, it will alert medical and security personnel that you have an implanted device.
The WATCHMAN Implant card has:
- Your name
- Your doctor’s name and phone number
- The model number of your implant
You might need your implant card if you get an MRI in the future.
The WATCHMAN Implant is “MR Conditional.” This means that it’s safe to have an MRI with the WATCHMAN Implant under specific conditions.
MRI conditions are set by device generation: the specific type of WATCHMAN Implant you have. This information is on your implant card. Show your implant card to your healthcare team so they can safely plan and provide an MRI.
Life with the WATCHMAN Implant
The WATCHMAN Implant can make it safer for you to enjoy the activities you once avoided due to the risk of bleeding from blood thinners. For many people, this may include things like hiking, gardening, and traveling without the constant worry of falls or injuries.
After you recover, you won’t feel or see the WATCHMAN Implant. It’s designed to stay in place permanently, offering lifelong protection from stroke caused by AFib. See what life is like with the WATCHMAN Implant.
Already took the quiz? Return to your personalized experience.
*In a clinical trial, 96% of patients were able to discontinue their blood thinner 45 days after getting the WATCHMAN Implant.
References:
- Kar, S., et al, Primary Outcome Evaluation of the Next Generation LAAC Device: Results from the PINNACLE FLX Trial, Circulation, 2021.
- Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61(2):755-759. doi:10.1016/0003-4975(95)00887-X
- CT Scan. Mayo Clinic website. https://www.mayoclinic.org/tests-procedures/ct-scan/about/pac-20393675 Accessed July 16, 2025.
- Echocardiogram: Transesophageal (TEE). Cleveland Clinic website. https://my.clevelandclinic.org/health/diagnostics/4992-echocardiogram-transesophageal-tee. Accessed July 16, 2025.
All images are the property of Boston Scientific. All trademarks are the property of their respective owners.
Content on this web page is for Informational Purposes only and does not constitute medical advice and should not be used for medical diagnoses. Boston Scientific strongly recommends that you consult with your physician on all matters pertaining to your health or to address any clinical/medical questions.
Important Safety Information
The WATCHMAN FLX and WATCHMAN FLX Pro Devices are permanent implants designed to close the left atrial appendage in the heart in an effort to reduce the risk of stroke.
With all medical procedures there are risks associated with the implant procedure and the use of the device. The risks include, but are not limited to, accidental puncture of the heart causing fluid to collect around the heart possibly leading towards the need for an additional procedure, allergic reaction, anesthesia risks, altered mental status or confusion after procedure, arrhythmias (irregular heartbeats), bleeding or throat pain from the TEE (Trans Esophageal Echo) probe, chest pain/discomfort, congestive heart failure, renal failure, excessive bleeding, gastrointestinal bleeding, groin puncture bleed, bruising at the catheter insertion site, groin pain, anemia (reduced red blood cells requiring transfusion), hypotension, infection/pneumonia (example: in or around your heart or lungs), misplacement of the device, improper seal of the appendage or movement of device from appendage wall, clot formation on the device, blood clot or air bubbles in the lungs or other organs, stroke, transient ischemic attack (temporary stroke-like symptoms), cranial bleed (bleeding in or around your brain), thrombosis (blockage of a blood vessel or vein by a clot) and in rare cases death can occur.
Be sure to talk with your doctor so that you thoroughly understand all of the risks and benefits associated with the implantation of the device. SH-2109508-AA

