A stroke can happen suddenly, but the risks build slowly and silently over time. Although stroke is one of the leading causes of death and disability in the United States, you can manage and reduce your risk.1,2 Did you know that people who have atrial fibrillation (AFib) have a five times higher risk of stroke than people with a regular heartbeat?3 In this article, we’ll walk through why strokes happen and what factors can increase your risk for having a stroke.
What happens during a stroke?
A stroke happens when blood flow to a part of the brain is suddenly cut off. The brain relies on a constant supply of oxygen-rich blood delivered through arteries that carry blood from the heart. If one of the arteries becomes blocked or bursts, blood can’t reach the brain tissue it normally supplies. Without a steady supply of oxygen-rich blood, brain cells will begin to die. Even a short disruption in blood flow can cause lasting damage in the brain.4,5
Depending on the part of the brain affected, a stroke can affect how you move, speak, or think. That’s why it’s so important to get medical care as soon as possible when a stroke occurs. 4,5
You may hear doctors refer to a stroke with different names, such as a brain attack or a cerebrovascular accident (also known as the medical abbreviation CVA). These terms all mean the same thing. 4,5

What causes a stroke?
A stroke happens when blood flow to part of the brain is interrupted, but there are different reasons why people have strokes. There are different types of strokes, each with its own cause. 4,5
Ischemic stroke
An ischemic stroke is the most common type of stroke. It accounts for about 87% of all strokes. During an ischemic stroke, a blood clot blocks one of the arteries providing blood to the brain. When the brain artery is blocked, it reduces blood flow (called ischemia).4-6
In some cases, a blood clot forms in a blood vessel inside the brain. This type of stroke is also called cerebral thrombosis or a thrombotic stroke. It’s most commonly caused by atherosclerosis (fatty deposits that build up on the artery wall). 4-6
In other cases, a blood clot forms in another part of the body, such as the heart. If the blood clot in the heart breaks off, it can travel through the bloodstream to the brain, where it gets stuck in a brain artery, cutting off the supply of oxygen-rich blood. This type of ischemic stroke is called a cerebral embolism or embolic stroke. AFib is the main cause of embolic strokes. 4-6
Hemorrhagic stroke
A hemorrhagic stroke happens when a blood vessel in the brain bursts and bleeds into the surrounding tissue. The leaking blood builds up in the area and compresses the surrounding brain tissue.4,5
Factors that can increase the risk of a hemorrhagic stroke include:5,7
- Uncontrolled high blood pressure, which can weaken blood vessel walls over time
- Blood thinners at high or unsafe levels, which can increase the risk of bleeding
- Bulges at weak spots in the wall of blood vessels in the brain, called aneurysms
- Head injury or trauma, which can cause bleeding in the brain
- Cerebral amyloid angiopathy, which causes protein deposits in the blood vessel wall
- Bleeding after an ischemic stroke
- Arteriovenous malformations (AVM), which is a tangle of abnormal blood vessels that can rupture and bleed
Transient ischemic attack
A transient ischemic attack is also known as a mini-stroke or by the medical abbreviation TIA. It happens when blood flow to the brain is temporarily blocked, usually for a few minutes. TIAs are usually caused by the same factors as an ischemic stroke, such as blood clots or atherosclerosis. However, in a TIA, the blood clot dislodges or dissolves on its own, making the effects temporary.4,5,8
Symptoms of a TIA usually only last a few minutes. However, TIAs are often a warning that a full-blown stroke could happen in the near future.
Who is at risk for a stroke?
A stroke can affect anyone, but some people have a higher risk than others. Most people who have strokes are older than 55 years. Men are more likely to have a stroke than women. However, when women have a stroke, they’re more likely to die than men.5,7
Your lifestyle habits can play a big role in your risk of stroke. Risk factors for stroke: 5,7
- Not getting enough physical activity
- Drinking alcohol
- Smoking or using other types of tobacco or vaping
- Using recreational drugs
Several health conditions can also increase the risk of stroke, such as: 5,7
- Overweight or obesity
- High blood pressure
- High cholesterol
- Diabetes
- Obstructive sleep apnea
- Heart disease, including AFib, heart failure, and heart defects
- Recent or ongoing COVID-19 infection
- Frequent migraine headaches
Your doctor can help you understand which risk factors for stroke you may have.
Why does AFib increase the risk of stroke?
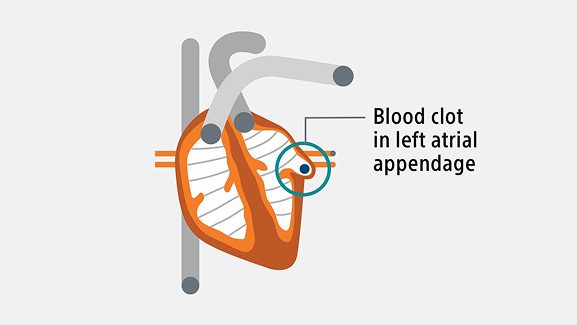
AFib is one of the medical conditions that can increase your risk of stroke. In AFib, the atria (the upper chambers of the heart) beat irregularly. This irregular rhythm prevents the heart from efficiently pumping blood out of the heart with each beat.9
The blood left behind in the heart can begin to pool, making it easier for blood cells to stick together and form blood clots. Blood clots often form in a small pouch in the atria called the left atrial appendage (LAA). If a blood clot escapes from the LAA, it can travel to the brain and cause an embolic stroke. 9
How to reduce stroke risk with AFib?
People with AFib are about five times more likely to have a stroke than those with a regular heartbeat.3 Reducing the risk of stroke is one the most important AFib treatments .10
Your doctor can use an assessment called the CHA2DS2-VASc risk to help decide if you need additional treatment to lower your stroke risk. This tool helps to estimate your chances of having a stroke by looking at different risk factors. These include your age, sex, and whether you have certain health conditions.11
Each factor is given a score. Your total will help your doctor decide what kind of stroke prevention you might need.
AFib treatments to lower the risk of stroke
If your risk of stroke is high, your doctor may recommend treatments to lower your risk. Blood thinner medications can help prevent the formation of blood clots. Taking blood thinners increases your risk of bleeding.11 Learn more about how blood thinners work.
Some people with non-valvular AFib who need an alternative to blood thinners may be eligible for a one-time procedure to close off the LAA, where most stroke-causing blood clots are formed.12,13 The WATCHMAN Implant is placed in a safe, minimally-invasive one-time procedure to close the LAA and reduce stroke risk – without the need for lifelong blood thinners.14
There are risks associated with all medical procedures. Please talk with your doctor about the risks and benefits of the WATCHMAN Implant.
Find out if you’re a candidate for the WATCHMAN Implant. Take the quiz
Healthy lifestyle habits
There are some stroke risk factors that you can’t control, like your age and sex. However, you can modify stroke risk factors related to your lifestyle habits, such as:15
- Eat a balanced diet
- Maintain a healthy weight
- Get regular physical activity
- Quit smoking
- Limit alcohol
- Manage health conditions that affect your risk of stroke, such as blood pressure, cholesterol, and diabetes
Healthy lifestyle changes are important for everyone, but they’re crucial for avoiding a stroke after a TIA.
How to recognize stroke symptoms
Stroke symptoms often come on suddenly. Recognizing stroke warning signs and getting help quickly can make a big difference in recovery.16
One way to remember the warning signs of a stroke is to use the acronym F.A.S.T.: 16
- F — face drooping
- A — arm weakness
- S — speech difficulty
- T — time to call 911
In addition to the F.A.S.T. signs, other common symptoms of a stroke can include: 16
- Numbness of part of the body, especially just on one side
- Confusion
- Difficulty seeing or vision changes
- Trouble walking or problems with balance and coordination
- Severe headache without a known cause
If you or a loved one experiences these symptoms, it’s important to act quickly. Every minute counts when someone is having a stroke.
Talk to your doctor about how you can prevent stroke
Someone in the United States has a stroke every 40 seconds.17 If you’re living with AFib, your risk of stroke is higher than those with a regular heart rhythm. It’s important to talk to your doctor about how to reduce your risk of stroke.
If you have non-valvular AFib and need an alternative to blood thinners to reduce your stroke risk, talk to your doctor about the WATCHMAN Implant.
Already took the quiz? Return to your personalized experience.
References:
- About stroke. American Heart Association website. Accessed July 18, 2025. https://www.stroke.org/en/about-stroke
- Bushnell C, Kernan WN, Sharrief AZ, et al. 2024 Guideline for the Primary Prevention of Stroke: A Guideline from the American Heart Association/American Stroke Association Stroke. 2024;55(12):e344-e424. doi:10.1161/STR.0000000000000475
- What is atrial fibrillation? American Heart Association website. Updated March 26,2025. Accessed March 26, 2025. July 18, 2025. https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af
- Explaining stroke. American Stroke Association website. Published 2020. Accessed July 18, 2025. https://www.stroke.org/en/-/media/Stroke-Files/Stroke-Resource-Center/Brochures/Explaining_Stroke_Brochure_2020.pdf?sc_lang=en
- Stroke. Cleveland Clinic website. Updated January 27, 2025. Accessed July 18, 2025. https://my.clevelandclinic.org/health/diseases/5601-stroke
- Ischemic stroke (clots). American Heart Association website. Accessed July 18, 2025. https://www.stroke.org/en/about-stroke/types-of-stroke/ischemic-stroke-clots
- Stroke. Mayo Clinic website. Updated December 13, 2024. Accessed July 18, 2025. https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113
- Transient ischemic attack (TIA). American Heart Association website. Accessed July 18, 2025. https://www.stroke.org/en/about-stroke/types-of-stroke/tia-transient-ischemic-attack
- Why atrial fibrillation matters. American Heart Association website. Updated May 26, 2025. Accessed July 18, 2025. https://www.heart.org/en/health-topics/atrial-fibrillation/why-atrial-fibrillation-af-or-afib-matters
- How are atrial fibrillation treatment options determined? American Heart Association website. Updated May 6, 2025. Accessed July 18, 2025. https://www.heart.org/en/health-topics/atrial-fibrillation/treatment-and-prevention-of-atrial-fibrillation/treatment-options-of-atrial-fibrillation-afib-or-af
- Atrial fibrillation medications. American Heart Association website. Updated May 14, 2025. Accessed July 18, 2025. https://www.heart.org/en/health-topics/atrial-fibrillation/treatment-and-prevention-of-atrial-fibrillation/atrial-fibrillation-medications
- Surgical procedures for atrial fibrillation. American Heart Association website. Updated May 6, 2025. Accessed July 18, 2025. https://www.heart.org/en/health-topics/atrial-fibrillation/treatment-and-prevention-of-atrial-fibrillation/surgical-procedures-for-atrial-fibrillation-afib-or-af
- Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61:755-759.
- Kar S., Doshi S., Sadhu A., et al. Primary Outcome Evaluation of the Next Generation LAAC device: Results from the PINNACLE FLX Trial. Circulation. 2021;143:1754–1762.
- Preventing stroke. Centers for Disease Control and Prevention website. Updated May 15, 2024. Accessed July 18, 2025. https://www.cdc.gov/stroke/prevention/index.html
- Stroke symptoms. American Heart Association website. Accessed July 18, 2025. https://www.stroke.org/en/about-stroke/stroke-symptoms
- Stroke facts. Centers for Disease Control and Prevention website. Updated October 24, 2024. Accessed July 18, 2025. https://www.cdc.gov/stroke/data-research/facts-stats/index.html
All images are the property of Boston Scientific. All trademarks are the property of their respective owners.
Content on this web page is for Informational Purposes only and does not constitute medical advice and should not be used for medical diagnoses. Boston Scientific strongly recommends that you consult with your physician on all matters pertaining to your health or to address any clinical/medical questions.
Important Safety Information
The WATCHMAN FLX and WATCHMAN FLX Pro Devices are permanent implants designed to close the left atrial appendage in the heart in an effort to reduce the risk of stroke.
With all medical procedures there are risks associated with the implant procedure and the use of the device. The risks include, but are not limited to, accidental puncture of the heart causing fluid to collect around the heart possibly leading towards the need for an additional procedure, allergic reaction, anesthesia risks, altered mental status or confusion after procedure, arrhythmias (irregular heartbeats), bleeding or throat pain from the TEE (Trans Esophageal Echo) probe, chest pain/discomfort, congestive heart failure, renal failure, excessive bleeding, gastrointestinal bleeding, groin puncture bleed, bruising at the catheter insertion site, groin pain, anemia (reduced red blood cells requiring transfusion), hypotension, infection/pneumonia (example: in or around your heart or lungs), misplacement of the device, improper seal of the appendage or movement of device from appendage wall, clot formation on the device, blood clot or air bubbles in the lungs or other organs, stroke, transient ischemic attack (temporary stroke-like symptoms), cranial bleed (bleeding in or around your brain), thrombosis (blockage of a blood vessel or vein by a clot) and in rare cases death can occur.
Be sure to talk with your doctor so that you thoroughly understand all of the risks and benefits associated with the implantation of the device. SH-2109508-AA

