About the procedure
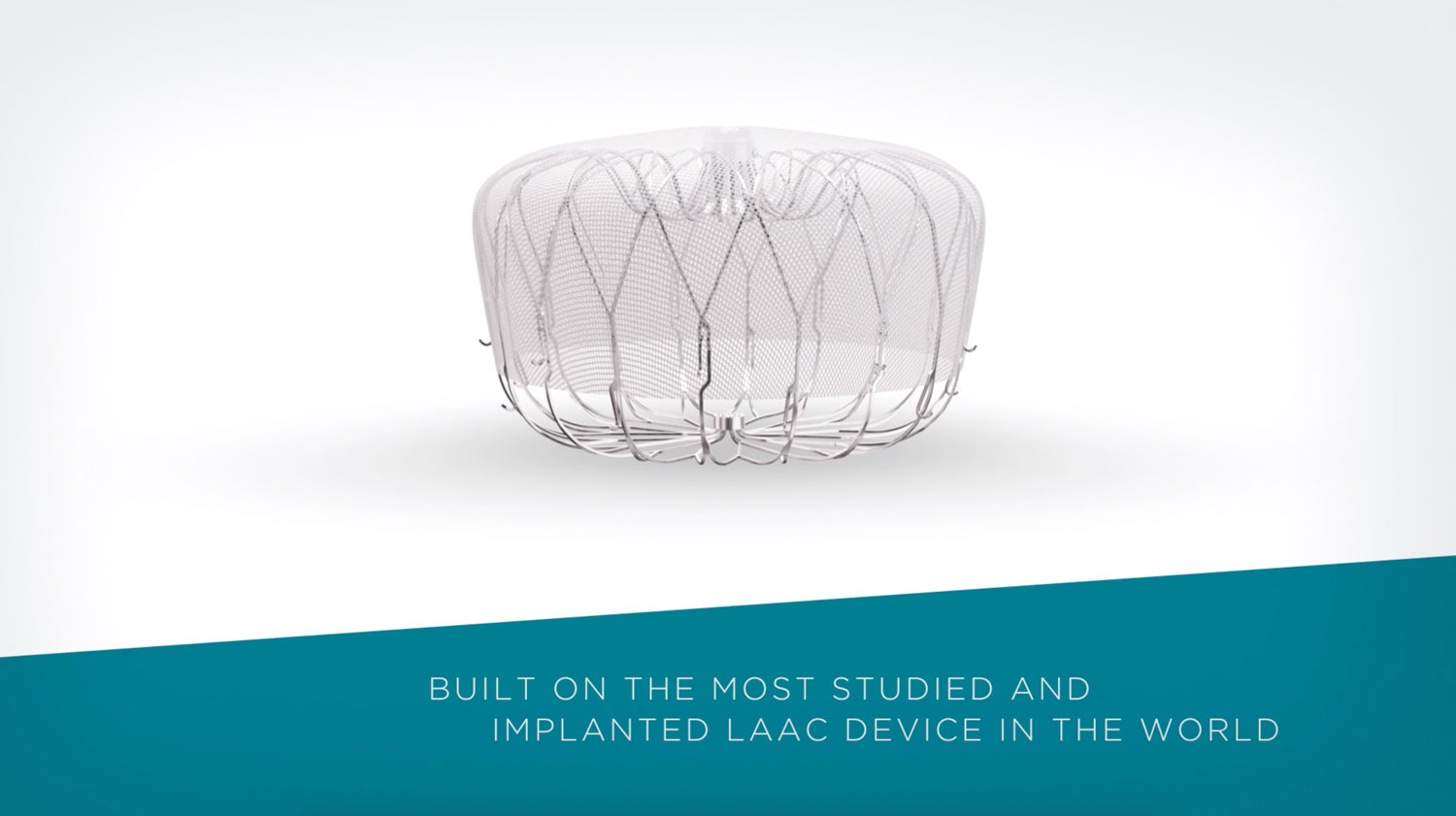
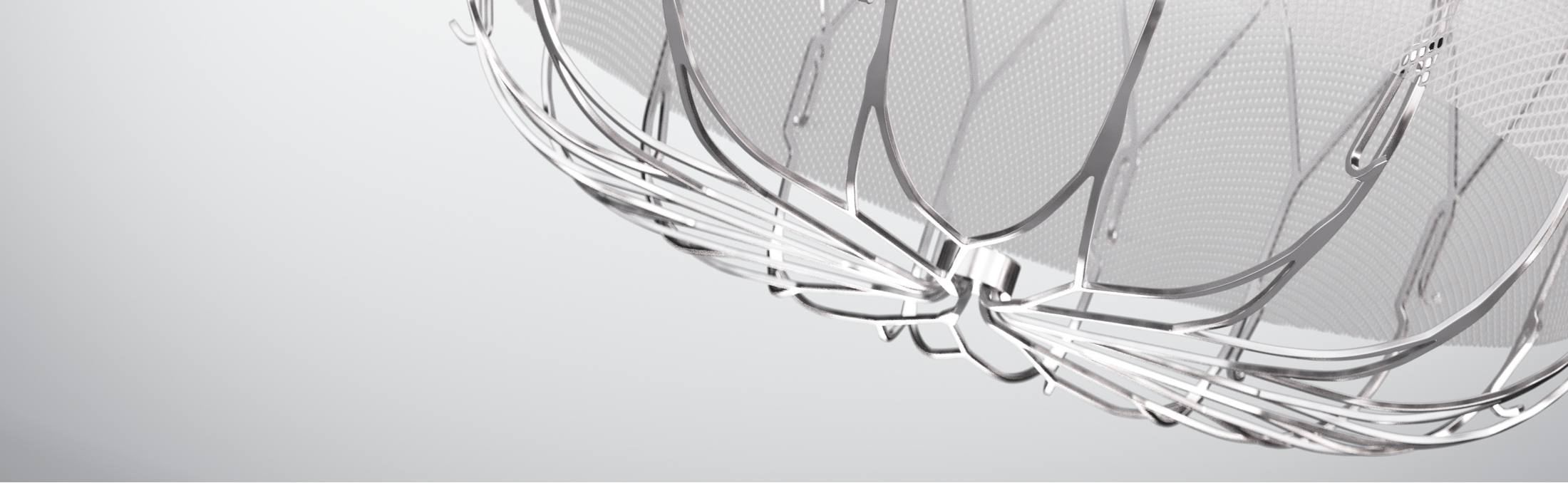
How WATCHMAN FLX works
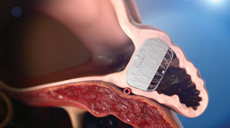
In non-valvular AF, >90% of stroke-causing clots that come from the left atrium are formed in the LAA1.
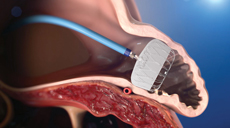
The WATCHMAN FLX LAAC Implant is a minimally invasive, one-time procedure designed to reduce the risk of strokes that originate in the left atrial appendage (LAA).

Minimally invasive

Permanent implant

Average hospital stay one day or less
WATCHMAN FLX LAAC procedure overview
WATCHMAN FLX Device receives FDA approval for DAPT labeling
With the approval of immediate DAPT-use post-implant, only the WATCHMAN FLX™ Implant provides you with flexibility to choose the ideal drug regimen that is best for your patient with clinical outcomes that support the safety and efficacy in preventing thrombosis and consequent stroke. Additionally, WATCHMAN FLX is the only LAAC device without a requirement of an overnight stay post procedure.
As always, you should exercise clinical judgment based on individual patient characteristics in determining the most appropriate use of anti-thrombotic drugs for the post-implant medication regimen.
Post-implant drug regimen options
At TEE, if leak >5mm, patients remain on OAC + ASA until seal is documented (leak <5mm)
*Any P2Y12 Inhibitor and Aspirin
WATCHMAN is implanted at top medical institutions across the country
- More than 650 major medical centers across the US are certified to implant WATCHMAN
- The WATCHMAN physician training program involves multiple phases including didactic training, imaging training, training in patient selection, device selection, complication management, and optional physician proctoring
- Individual physicians and/or the collective physician-team must be proficient in transseptal skills prior to entering the WATCHMAN training program
References:
- Blackshear JL., Odell JA. Annals of Thoracic Surg. 1996; 61: 755-759.
- Kar, S., et al, Primary Outcome Evaluation of the Next Generation LAAC Device: Results from the PINNACLE FLX Trial, Circulation, 2021.